Personalized Medicine: Customizing Treatments Based on Genetics
“Unlocking the Genetic Code: How Personalized Medicine is Revolutionizing Healthcare”
Key takeaways:
- Personalized medicine tailors treatments to individuals based on their genetics.
- Genomics is essential for identifying genetic factors in diseases.
- Targeted therapies revolutionize cancer treatment.
- Pharmacogenomics optimizes drug response through genetics.
- Personalized medicine extends to various diseases beyond cancer.
- Artificial Intelligence aids in genomic analysis and treatment predictions.
- Regulatory and economic challenges impact personalized medicine adoption.
- The future holds promising advancements in technology and healthcare integration.
In the ever-evolving landscape of modern medicine, a groundbreaking approach has emerged, offering hope and potential like never before – Personalized Medicine. At the heart of this medical revolution lies a deep understanding of genetics, unlocking the key to tailoring treatments precisely to each individual’s unique genetic makeup. Gone are the days of the one-size-fits-all approach; instead, a new era is dawning, where medical care is finely tuned to match the distinct needs of patients. This article delves into the fascinating realm of Personalized Medicine, exploring its promise, the pivotal role genetics plays in treatment, and the remarkable journey that has transformed medicine from a broad brush to a precise, personalized canvas. As we journey through this transformative realm, we will witness the immense potential and remarkable achievements of Personalized Medicine, revolutionizing healthcare and paving the way toward a future of better patient outcomes and increased well-being.
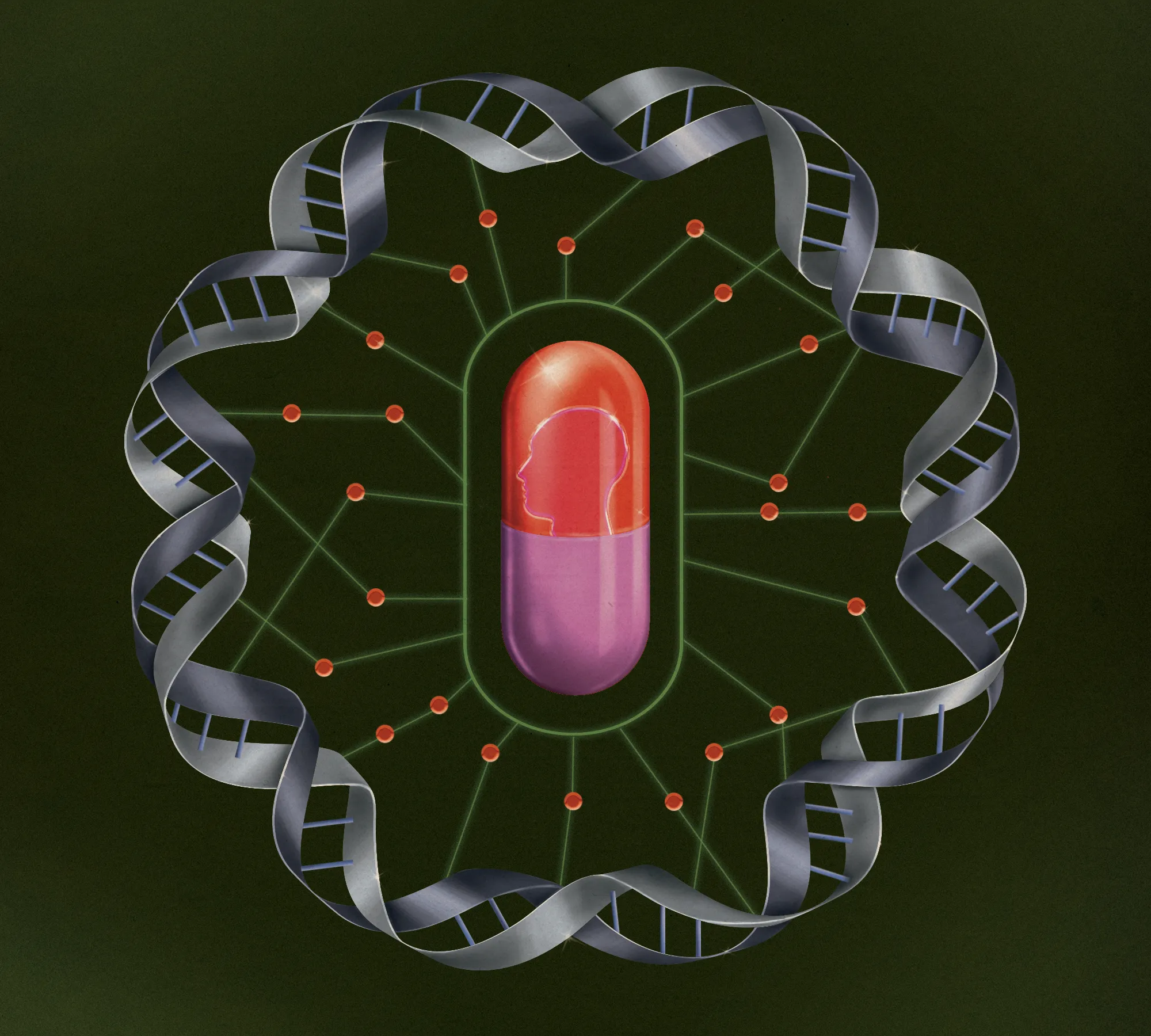
To comprehend the profound impact of Personalized Medicine, one must first grasp the pivotal role of genetics in shaping an individual’s health and response to treatment. The human genome, a complex tapestry of genetic information, holds the key to unlocking the mysteries of disease susceptibility and treatment efficacy. Within this intricate code lie variations and mutations that can influence how our bodies process medications, respond to therapies and even determine our predisposition to certain illnesses.
Genetic testing, a fundamental component of Personalized Medicine, has become increasingly accessible and sophisticated, enabling healthcare providers to delve deep into a patient’s DNA to identify specific genetic markers. These markers offer crucial insights into the individual’s risk factors, potential treatment responses, and susceptibility to adverse drug reactions. Armed with With this knowledge, medical professionals can tailor treatments with unrivaled precision, maximizing therapeutic benefits while minimizing the risk of adverse events.
Beyond hereditary diseases, genetics also plays a critical role in understanding complex conditions such as cancer, cardiovascular disorders, and neurological diseases. By identifying the genetic drivers behind these ailments, researchers and clinicians can develop targeted therapies that directly address the root cause of the illness. This concept was once deemed unimaginable in traditional medicine.
The transition from a one-size-fits-all medical approach to Personalized Medicine is revolutionary. General principles and extensive treatment protocols that aimed to benefit the typical patient were the foundation for medical practices for centuries. While this approach has undoubtedly saved countless lives and alleviated widespread suffering, it has left many individuals with unanswered questions and unresolved health issues.
In the early 21st century, advances in technology and the Human Genome Project laid the foundation for a paradigm shift in medicine. The groundbreaking endeavor to map the entire human genome provided scientists with an invaluable blueprint to decode the intricate genetic architecture of humanity. This milestone discovery opened the floodgates to an era of personalized care, where each person’s genetic makeup became a treasure trove of information guiding medical decisions.
As genetic testing became more accessible and affordable, the possibilities of Personalized Medicine began to flourish. Researchers, clinicians, and pharmaceutical companies united in pursuing innovative treatments tailored to the individual, and the results were nothing short of extraordinary. Targeted therapies emerged, offering newfound hope to patients with rare diseases previously deemed untreatable.
Genomics: The Foundation of Personalized Medicine
In pursuing a new era of healthcare, personalized medicine has emerged as a transformative approach, offering tailor-made treatments to match each individual’s unique genetic blueprint. Genomics is at the heart of this medical revolution – the study of an individual’s complete set of genes. Decoding the human genome has unveiled a treasure trove of genetic information, allowing researchers and clinicians to identify variations, mutations, and genetic markers that shape our health and response to treatments. This article explores the foundational role of genomics in personalized medicine and its applications in targeted therapies, pharmacogenomics, personalized cancer treatments, and beyond. H2: II. Genomics: The Foundation of Personalized Medicine
Decoding the Human Genome
The Human Genome Project, a monumental scientific endeavor completed in 2003, marked a defining moment in the field of genomics. This groundbreaking project aimed to map and sequence all the genes in the human genome, unraveling the unique genetic code that defines each individual. With the completion of this ambitious feat, researchers gained an unprecedented understanding of our genetic composition, which comprises over three billion nucleotide base pairs.
Decoding the human genome laid the foundation for personalized medicine, as it allowed scientists to identify and catalog the entire set of genes responsible for an individual’s physical traits and biological functions. Through this comprehensive knowledge of our genetic makeup, medical practitioners can now navigate the intricate pathways of disease susceptibility, ultimately guiding the development of personalized treatment plans.
Identifying Genetic Variations and Mutations
Genetic variations and mutations are inherent to the diversity of the human population. These variations can influence how our bodies metabolize medications, respond to therapies, and interact with the environment. Identifying these genetic variations in personalized medicine is paramount to delivering effective and safe treatments.
Researchers have made remarkable strides in characterizing various genetic variations and mutations that can increase or decrease an individual’s risk of developing certain diseases. By studying these genetic markers, medical professionals can tailor interventions and preventative measures, allowing for early detection and proactive healthcare management.
Importance of Genetic Testing in Personalized Medicine
Genetic testing has emerged as a cornerstone of personalized medicine, offering insights into an individual’s unique genetic profile. By analyzing a patient’s DNA, healthcare providers can identify specific genetic markers linked to various diseases and conditions, enabling the early detection of potential health risks. This proactive approach facilitates timely and targeted interventions, ensuring patients receive treatments tailored to their needs.
Targeted Therapies: Precision Medicine in Action
Tailoring Treatments to Specific Genetic Markers
One of the most significant achievements of personalized medicine is the development of targeted therapies that hone in on specific genetic markers associated with particular diseases. Unlike traditional treatments that often take a broad approach, targeted therapies are designed to address the molecular and genetic abnormalities driving a patient’s illness. By precisely targeting these underlying causes, targeted therapies can be more effective, with fewer side effects than conventional treatments.
Through genomic profiling, clinicians can identify genetic mutations or alterations characteristic of certain diseases, such as specific types of cancer. With this knowledge, researchers can design medications or treatments that selectively attack the aberrant cells, leaving healthy cells largely unharmed. This approach has proven highly successful in treating conditions like breast cancer, lung cancer, and leukemia, where patients have experienced improved outcomes and extended survival rates.
Advancements in Targeted Therapy Research
The field of targeted therapy research continues to evolve rapidly, driven by groundbreaking discoveries in genomics and molecular biology. As technology advances, researchers can now analyze vast amounts of genomic data faster and more accurately. This has led to identifying new genetic targets and the development of innovative therapies across various medical disciplines.
For instance, researchers are exploring ways to harness the body’s immune system to target cancer cells based on their genetic features, specifically in immunotherapy. Immunotherapies have shown remarkable success in patients with advanced melanoma, kidney cancer, and certain lymphomas. Moreover, the ongoing research in targeted therapies extends beyond cancer, showing promise in treating other diseases with genetic underpinnings, such as cystic fibrosis, rheumatoid arthritis, and rare genetic disorders.
Success Stories of Targeted Therapies
The success stories of targeted therapies offer shining examples of how personalized medicine transforms patient outcomes. One of the most celebrated examples is the development of Imatinib, a targeted therapy revolutionizing the treatment of chronic myeloid leukemia (CML). Imatinib, also known by its trade name Gleevec, specifically targets the abnormal protein produced by the BCR-ABL gene fusion, which drives the growth of CML cells. Imatinib has led to remarkable remission rates by inhibiting this unique genetic driver and has turned CML from a fatal diagnosis into a manageable chronic condition.
Another inspiring success story is the use of Herceptin (Trastuzumab) in the treatment of HER2-positive breast cancer. HER2 is a specific protein found on the surface of some breast cancer cells. Herceptin is a targeted therapy that precisely targets and blocks HER2, effectively slowing down cancer growth and reducing the risk of recurrence. The introduction of Herceptin has significantly improved the prognosis for HER2-positive breast cancer patients, increasing survival rates and quality of life.
Pharmacogenomics: Optimizing Drug Response
How Genetics Influence Drug Metabolism
Pharmacogenomics, the study of how genetics influence an individual’s response to medications, is a game-changer in personalized medicine. Our genetic makeup can significantly impact how our bodies metabolize and respond to drugs, leading to variations in drug efficacy and potential side effects. Understanding these genetic factors is paramount to optimizing drug therapy, and tailoring treatments to each patient’s unique genetic profile.
Enzymes in the liver play a crucial role in metabolizing drugs, and the genes responsible for these enzymes can vary between individuals. Genetic variations in these enzymes can lead to differences in drug clearance rates, affecting how quickly or slowly drugs are broken down and eliminated from the body. Such variations can result in individuals being classified as “fast metabolizers” or “slow metabolizers,” influencing the dosage and frequency of medication needed to achieve the desired therapeutic effect.
Individual Variability in Drug Response
Individual variability in drug response is a common phenomenon observed in clinical practice. Some patients may experience excellent results with a standard medication dose, while others may not respond as expected or experience adverse reactions. Pharmacogenomics provides insights into these individual differences, explaining varying responses and guiding healthcare providers in making informed decisions about drug selection and dosing.
For example, the drug Warfarin, commonly used as a blood thinner, is known to have a narrow therapeutic range, meaning that the difference between an effective dose and a harmful dose is relatively small. Genetic testing can identify variations in the CYP2C9 and VKORC1 genes, influencing how Warfarin is metabolized and its effectiveness as an anticoagulant. By considering an individual’s genetic profile, healthcare providers can tailor Warfarin dosages more precisely, reducing the risk of bleeding complications while maintaining the desired therapeutic effect.
Implementing Pharmacogenomics in Clinical Practice
Integrating pharmacogenomics into clinical practice is vital in harnessing its potential to enhance patient outcomes. As genetic testing becomes more accessible and affordable, healthcare providers increasingly incorporate pharmacogenomic testing into routine patient care. By analyzing a patient’s genetic profile, clinicians can identify potential drug interactions, predict adverse drug reactions, and optimize medication choices.
Pharmacogenomic guidelines are being developed and updated regularly to aid healthcare providers in making evidence-based decisions. These guidelines help clinicians interpret genetic testing results and provide recommendations on drug dosing adjustments based on a patient’s genetic profile. Moreover, electronic health record (EHR) systems are designed to include pharmacogenomic information, ensuring that healthcare providers can access this critical data during medication prescribing and administration.
Personalized Cancer Treatments: Breakthroughs in Oncology
Genomic Profiling for Cancer Patients
Personalized cancer treatments have brought newfound hope to patients facing this formidable disease. At the forefront of this revolution is genomic profiling, a process that involves analyzing the genetic makeup of a tumor to identify specific genetic alterations driving its growth. By understanding the unique genetic characteristics of each patient’s cancer, oncologists can design targeted therapies that directly address the molecular drivers of the disease.
Genomic profiling enables oncologists to classify cancers more precisely, guiding treatment decisions and predicting how tumors may respond to different therapies. For example, breast cancer is not a singular disease but a heterogeneous group of tumors with distinct genetic subtypes. By identifying specific genetic markers in a breast cancer patient’s tumor, clinicians can prescribe treatments tailored to that subtype, leading to better outcomes and potentially sparing patients from unnecessary side effects associated with less targeted treatments.
Immunotherapy and Cancer Vaccines
Immunotherapy has emerged as a groundbreaking approach in personalized cancer treatments, leveraging the body’s immune system to target and destroy cancer cells. Unlike traditional treatments like chemotherapy and radiation, which broadly target rapidly dividing cells, immunotherapy aims to boost the immune system’s ability to recognize and eliminate cancer cells.
Checkpoint inhibitors are one of the most prominent types of immunotherapy. These drugs block specific molecules that suppress the immune system’s response, essentially “releasing the brakes” and allowing immune cells to attack cancer cells more effectively. Clinical trials have shown remarkable success in treating advanced melanoma, lung cancer, and other malignancies with checkpoint inhibitors, leading to durable responses and prolonged survival for some patients.
Cancer vaccines, another avenue of personalized cancer treatments, train the immune system to recognize and attack cancer cells. These vaccines are developed using a patient’s tumor-specific antigens, unique to their cancer cells. The vaccine primes the body to recognize and mount an immune response against the cancer by exposing the immune system to these antigens. Although cancer vaccines are still in the early stages of development, they hold tremendous promise as a personalized approach to cancer prevention and treatment.
Challenges and Future Directions in Personalized Cancer Care
While personalized cancer treatments have shown remarkable success, they also present challenges that researchers and clinicians must address. One of the significant challenges lies in identifying suitable genetic targets for all cancer types. Some cancers may have few actionable genetic mutations, limiting the availability of targeted therapies. Expanding the knowledge of cancer genomics and developing novel targeted therapies remains an ongoing pursuit in oncology.
Furthermore, the high cost of personalized cancer treatments and genetic profiling can hinder equitable access. As the field advances, efforts to make these treatments more accessible and affordable to all patients will be crucial.
Beyond Cancer: Personalized Medicine in Other Diseases
Cardiovascular Diseases and Genetic Predisposition
Cardiovascular diseases, including heart disease and stroke, are among the leading causes of death worldwide. Genomics has shed light on the genetic predisposition to these diseases, revealing that certain genetic variations can increase an individual’s risk of developing cardiovascular conditions. By identifying these genetic risk factors, healthcare providers can implement targeted preventive measures and early interventions to mitigate the risk of heart disease.
For instance, genetic testing can uncover specific genetic markers associated with familial hypercholesterolemia, a genetic disorder that leads to dangerously high cholesterol levels. With this knowledge, physicians can initiate aggressive cholesterol-lowering treatments early on, significantly reducing the likelihood of heart attacks and strokes in affected individuals.
Neurological Disorders and Precision Treatments
Neurology has also made significant advances in personalized medicine, particularly in the understanding and treatment of neurological disorders. Conditions such as Alzheimer’s disease, Parkinson’s disease, and amyotrophic lateral sclerosis (ALS) have complex genetic underpinnings, making each patient’s experience unique. Genomic studies have uncovered rare genetic variants linked to some neurological disorders, and this knowledge is paving the way for personalized treatments and therapeutic interventions.
In some cases, genetic testing can help diagnose these conditions earlier, enabling proactive disease management and potential therapeutic interventions to slow disease progression. Furthermore, clinical trials are exploring gene therapies and other personalized approaches in treating genetic neurodegenerative diseases, offering hope for the future of neurology.
Autoimmune Diseases and Personalized Therapies
Autoimmune diseases, where the immune system mistakenly attacks the body’s tissues, affect millions of people worldwide. The intricate interplay between genetics and the immune system plays a central role in these disorders. Through genomic studies, researchers have uncovered genetic variants associated with various autoimmune diseases, including rheumatoid arthritis, multiple sclerosis, and type 1 diabetes.
Personalized medicine transforms the management of autoimmune diseases by guiding treatment choices based on a patient’s genetic profile. For instance, in rheumatoid arthritis, genetic testing can help identify individuals more likely to respond well to specific biologic medications, sparing them from a trial-and-error approach and potential side effects of ineffective treatments.
As genomics and personalized medicine research advances, we can expect even more breakthroughs and applications in various medical specialties. The knowledge gained from genomic studies revolutionizes how we understand and treat diseases, providing a glimpse into a future where healthcare is tailored to each individual’s unique genetic makeup.
Ethical and Privacy Considerations in Personalized Medicine
As personalized medicine becomes more prevalent in healthcare, it brings important ethical and privacy considerations. The use of genetic data raises questions about patient consent, data ownership, and the potential for discrimination based on genetic information.
Informed consent is critical when conducting genetic testing and using genomic data for personalized treatments. Patients should fully understand the implications of genetic testing, including the potential implications for themselves and their families. Transparent communication between healthcare providers and patients is essential to ensuring that patients can make informed decisions about genetic testing and using their genetic data.
Safeguarding genetic data and patient confidentiality is paramount. As genetic information can reveal sensitive and private information about an individual and their family, strict measures must be in place to protect this data from unauthorized access or misuse. Health institutions and researchers must adhere to robust privacy regulations and data security protocols to maintain patient trust and confidentiality.
Ensuring equitable access to personalized medicine is also a critical ethical consideration. As genetic testing and personalized treatments can be costly, efforts must be made to make these advancements accessible to all patients, regardless of their socioeconomic status or geographic location. Addressing disparities in access to personalized medicine is essential to ensuring that the benefits of genomic advancements are available to everyone.
VIII. The Role of Artificial Intelligence in Personalized Medicine
Leveraging AI for Genomic Analysis
The vast amount of genomic data generated through genetic testing requires powerful tools to make sense of it all. This is where artificial intelligence steps in, revolutionizing genomic analysis and interpretation. AI algorithms can sift through massive genomic datasets at incredible speeds, identifying genetic variations, mutations, and markers associated with diseases. By detecting patterns and correlations that may be invisible to the human eye, AI helps researchers and clinicians uncover valuable insights for personalized medicine.
AI-powered genomic analysis is pivotal in diagnosing rare genetic disorders, predicting disease risk, and tailoring treatment plans. In complex diseases like cancer, AI algorithms can precisely categorize subtypes of tumors based on genetic signatures, guiding oncologists in selecting targeted therapies that are most likely effective. The synergy between AI and genomics accelerates medical discoveries, propelling personalized medicine into uncharted territory.
Predictive Analytics and Treatment Recommendations
With unparalleled precision, AI-powered predictive analytics enables personalized medicine to forecast patient outcomes and suggest treatment plans. AI algorithms can identify patient-specific patterns that inform tailored interventions by analyzing vast patient data, including medical history, genetics, lifestyle factors, and responses to previous treatments.
For instance, AI-driven predictive models can assess a patient’s response to a medication based on their genetic profile and clinical characteristics. This information enables clinicians to make informed decisions about drug dosages and medication choices, reducing the risk of adverse reactions and enhancing treatment efficacy. AI algorithms can predict patient deterioration in critical care settings, allowing medical teams to intervene proactively and prevent adverse events.
AI Challenges and Its Potential in Healthcare
As AI continues to shape personalized medicine, it also brings challenges that must be addressed to realize its potential fully. One of the primary concerns is data privacy and security. The integration of AI requires access to vast amounts of sensitive patient data, raising ethical questions about data ownership, consent, and protection. Healthcare institutions and AI developers must prioritize robust data security measures to safeguard patient information and maintain trust in the healthcare system.
Another challenge lies in the interpretability and transparency of AI algorithms. In personalized medicine, clinicians must understand how AI arrives at its treatment recommendations and predictions. Transparent and interpretable AI models are vital to fostering clinician confidence in AI-driven decision-making aensuringure they can effectively collaborate with these technologies in patient care.
Furthermore, AI implementation requires significant infrastructure investment, computational resources, and specialized expertise. Healthcare organizations must embrace digital transformation and provide adequate training to clinicians and staff to harness the full potential of AI.
Regulatory and Economic Challenges for Personalized Medicine
FDA and Approval of Personalized Treatments
The development and approval of personalized treatments pose unique challenges for regulatory agencies like the U.S. Food and Drug Administration (FDA). Traditional drug approval processes are often designed for large populations with one-size-fits-all treatments. In contrast, personalized medicine focuses on smaller patient groups with specific genetic markers or rare conditions.
To address these challenges, regulatory agencies are adapting their frameworks to accommodate personalized medicine. The FDA has established pathways for accelerated approval of targeted therapies based on robust evidence of efficacy and safety in specific patient subsets. Biomarker-driven clinical trials play a crucial role in gathering the necessary data to support the approval of personalized treatments.
Reimbursement and Cost-effectiveness
The economic aspect of personalized medicine raises questions about reimbursement and cost-effectiveness. Personalized treatments, especially those developed for smaller patient populations, may have higher development and manufacturing costs. Additionally, genetic testing and AI-driven analyses can add to the overall expenses of personalized medicine.
Healthcare systems and insurers must navigate the delicate balance of providing access to innovative and effective treatments while ensuring the affordability and sustainability of healthcare services. Demonstrating the cost-effectiveness and long-term benefits of personalized medicine becomes essential in securing reimbursement and making these treatments more accessible to patients.
Overcoming Barriers to Widespread Adoption
The widespread adoption of personalized medicine faces obstacles related to technology integration, data sharing, and clinician training. Healthcare institutions must invest in advanced technologies and infrastructure to support AI-driven personalized medicine. The interoperability of electronic health record systems is crucial for seamless data sharing and collaboration between healthcare providers.
Moreover, effective clinician training and education are essential for successfully integrating personalized medicine and AI tools into clinical practice. Healthcare professionals must be well-versed in genomic analysis, AI algorithms, and the interpretation of complex data to leverage these tools for patient care effectively.
Despite these challenges, the potential benefits of personalized medicine and AI in healthcare are vast. Delivering precise and targeted treatments can improve patient outcomes, reduce healthcare costs, and enhance patient satisfaction.
The Future of Personalized Medicine
Advancements in Technology and Research
As technology continues to advance, so does the potential for personalized medicine. Emerging genomic sequencing technologies, faster computing power, and AI algorithms will continue to propel research and innovation in this field. The ability to analyze massive datasets quickly and accurately will open new avenues for understanding disease mechanisms and identifying novel therapeutic targets.
Integration of Personalized Medicine into Healthcare Systems
Integrating personalized medicine into healthcare systems will become more seamless as AI technologies and genetic testing become standard practice. Electronic health record systems will be equipped to store and analyze genetic data, enabling real-time decision support for personalized treatment recommendations. Clinicians will have access to comprehensive patient profiles that include genetic information, allowing them to tailor treatments based on each patient’s unique characteristics.
Transforming Medicine for Better Patient Outcomes
The ultimate goal of personalized medicine is to improve patient outcomes and quality of life. With AI-driven predictive analytics and treatment recommendations, clinicians can make more informed decisions, leading to more precise and effective treatments. Personalized medicine will revolutionize how diseases are diagnosed, managed, and treated, empowering patients with customized care plans targeting the root cause of their illnesses.
Conclusion
Personalized medicine using artificial intelligence holds the potential to revolutionize patient care as we stand on the verge of a transformative era in healthcare. By leveraging AI for genomic analysis, predictive analytics, and treatment recommendations, we can unlock the full potential of personalized medicine and bring forth a new age of precision healthcare. Despite challenges in regulatory and economic aspects, integrating personalized medicine into mainstream healthcare systems is on the horizon, paving the way for better patient outcomes, enhanced disease management, and a future where healthcare is truly tailored to the individual. Embracing personalized medicine and AI technologies is a leap towards enhanced healthcare but also a testament to the remarkable potential of human ingenuity in shaping a healthier and more resilient future.
The landscape of contemporary healthcare is changing thanks to personalized medicine and the transformative power of genomics. From targeted therapies and pharmacogenomics to breakthroughs in oncology and managing various diseases, the integration of genetic insights is revolutionizing how we prevent, diagnose, and treat illnesses. Technological advancements and a better understanding of the human genome drive the ongoing journey of personalized medicine. As we navigate this remarkable frontier, the potential for better patient outcomes and a more equitable, personalized healthcare future shines brighter.